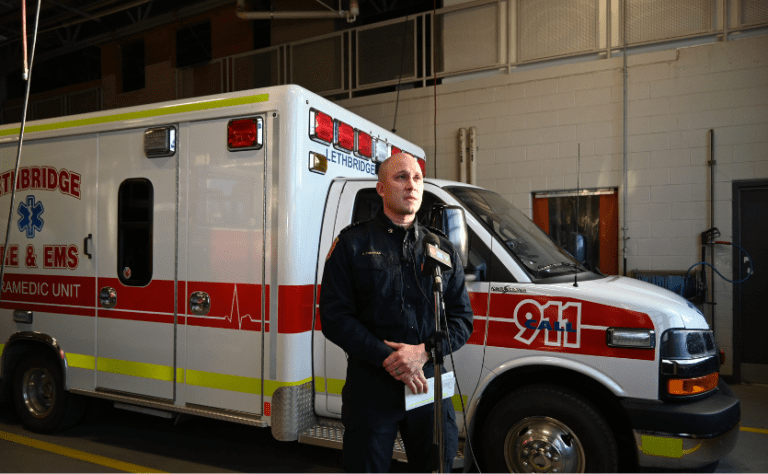
The City of Lethbridge Fire and Emergency Services has been navigating challenges with fleet renewal amidst increasing operational demands. With 20 years of experience in the field, both Christopher Tomaras, Deputy Chief of Operations, and Mike Humphrey, EMS Operations Officer, have witnessed the growing strain on emergency services, especially with the increasing call volume. A pivotal part of their fleet management strategy has been incorporating ambulance remounts to address fleet renewal while ensuring operational efficiency.

Fleet Renewal Strategy: Remounting Saves Money
Serving a population of about 100,000 people in Southern Alberta, Lethbridge’s fleet, now composed of 14 active ambulances has evolved over the years. Today, ambulances are expected to meet a higher standard as they bear an increasing operational load. “We expect a lot more out of the apparatus, and we’re putting a lot more miles on these units,” explains Christopher Tomaras. The growing demand for emergency services has spurred LFES to take proactive measures. In response, the remount process is now integral to LFES’s fleet renewal strategy.
The Service has adopted a system where ambulances are remounted after four years. After eight years, the entire unit is typically replaced. As Mike Humphrey puts it, “By using this strategy, we were able to decrease the lifecycle of an ambulance from 6-7 years to four years, and use the savings to get additional resources, like stretchers, without compromising the quality of service.” This strategy has not only helped reduce costs but has also allowed LFES to maintain a more responsive and efficient fleet while better-addressing community needs.
In an interview given to local media, Chris Tomaras also emphasized that this practice “reduces waste and helps us stay sustainable. This lets us keep our fleet modern and save taxpayer money”. The article notes that “new ambulances typically cost around $282,000. The cost to remount it onto a new chassis, or base frame of the vehicle, is about $88,000, or 31 %, cheaper.”
According to Christopher Tomaras, the remount process has been extremely valuable in ensuring fleet reliability without the long delays often seen with new builds. “Once those chassis do come in, it’s about a four to six-week turnaround versus the time of a full build on a new ambulance,” he explains.
Positive Feedback from Frontline Workers
Despite having only two remounted units currently in service (with three more expected in the coming months), the feedback has been positive overall. “They’re just as good, if not the same, as a new build,” shares Tomaras. The paramedics’ input confirms that the remounted vehicles meet the operational needs just as effectively. The units offer well-organized storage compartments, accessible medical equipment, and a functional layout—features that are crucial for providing high-quality patient care.
Additionally, the vehicles are structurally sound, equipped with up-to-date technology, and have all the safety features required to ensure paramedics’ ability to respond confidently to emergency situations. “We’re not having buyer’s remorse,” adds Humphrey, underscoring the overall satisfaction with the remount process.
Addressing the Challenges of Ambulance Availability
However, the key challenge remains not the functionality of the remounts, but the availability of new ambulances, which have become harder to secure due to prolonged delivery times. LFES frequently faces pressure to keep their vehicles in service, sometimes with no backup ambulances available. “We’ve been lucky. We’ve run multiple days where we have zero ambulances in reserve”, Tomaras noted.

Looking to Other Options
While the remount process has been a key component of LFES’s strategy, the department is also exploring other potential solutions to address future fleet needs. They are considering transitioning to a truck chassis, which is easier for fleet services to maintain. As for the patient compartment, paramedics always have a say in its layout. “We choose our options based on feedback from frontline staff,” emphasized Humphrey, so they can choose what works best for both the paramedics and the patients.